Clinical evaluation and instrumental diagnostics in acute acromioclavicular joint dislocation
Complete and timely early diagnosis of acromioclavicular dislocation allows for a differentiated approach to surgical treatment tactics, preventing possible complications and restoring the function of the injured shoulder joint to the fullest extent.
Published: 05.04.2024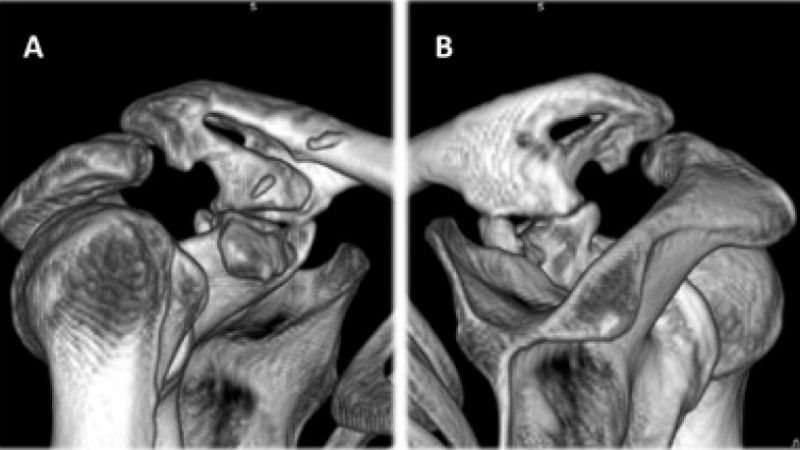
Clinical evaluation and instrumental diagnostics in acute acromioclavicular joint dislocation
Serhii Bezruchenko (1), Oleksii Dolhopolov (1), Maryna Yarova (1), Roman Luchko (2), Vadim Mazevych (2)
1 Scientific, Organization and Methodology Department, SI “Institute of Traumatology and Orthopedics of the NAMS of Ukraine”, Kyiv, Ukraine
2 Functional Diagnostics Department SI “Institute of Traumatology and Orthopedics of the NAMS of Ukraine,” Kyiv, Ukraine
SUMMARY
Background. The aim was to improve the diagnosis of acromioclavicular joint dislocation by studying the capabilities and characteristics of clinical and instrumental diagnostic methods. The idea is expressed that modern clinical and instrumental diagnostic methods comprise a large number of techniques, but no single algorithm for diagnosing injury to the AC joint has been developed. A gold standard for investigating and diagnosing acute AC joint dislocation does not currently exist.
Materials and Methods. A retrospective study of the characteristics and capabilities of clinical and instrumental diagnostic methods was performed in 152 patients with traumatic shoulder pathology. The patients were divided into two groups: Group I of 102 patients (67%) with acromioclavicular joint dislocation type III-VI according to Rockwood classification and Group II of 50 patients (33%) with a partial tear of the rotator cuff. Clinical and instrumental examinations involved specific provocative tests; the radiological diagnostics comprised conventional radiographs with the Zanca, axillary and Alexander views, and CT, MRI, and ultrasound examinations.
Results. The characterization of examination methods was based on the records of patients in Group I and II. The most sensitive clinical test to establish Rockwood type V of acromioclavicular joint dislocation was the Paxinos test (91%). The lowest sensitivity across the tests used was observed with the active compression test to diagnose type IV of dislocation (50%). As regards the X-ray examination, the axial view was 100% sensitive for detecting type IV and VI AC joint dislocation. The Zanca view is highly sensitive for patients with Rockwood type V and Alexander view for Rockwood type III and V dislocations. The accuracy of ultrasound work-up in Group I was 95%, with 96% sensitivity and 93% specificity, while MRI accuracy was 97%, with 96% sensitivity and 98% specificity, and CT accuracy was 81%, with 83% sensitivity and 75% specificity.
Conclusions. 1. Determination of the sensitivity and specificity of the X-ray examination revealed the absence of a 100% effective X-ray view for type III and V AC joint dislocation. 2. The accuracy and sensitivity of the ultrasound, MRI, and CT examinations are high. 3. There is currently no consensus on a protocol to view acute AC joint injuries. 4. Complete and timely early diagnosis of acromioclavicular dislocation allows for a differentiated approach to surgical treatment tactics, preventing possible complications and restoring the function of the injured shoulder joint to the fullest extent.
Key words: diagnostics, sensitivity and specificity, acromioclavicular joint, MRI, outcomes
BACKGROUND
The acromioclavicular (AC) joint is one of the most commonly injured joints of the upper extremity, taking third place after shoulder and elbow joint dislocation [1]. The estimated incidence of injuries of the AC joint in the general population is 3–4 per 100,000 population per year [2]. The male-female ratio is as high as 8:1; many injuries are associated with the promotion of a healthy lifestyle among the population between the ages of 20 and 40 years [3]. The AC joint is a key component of the shoulder girdle, which provides a connection between the upper extremity and the axial skeleton [4]. AC joint dislocation causes injury to the capsular ligaments (superior, inferior, anterior, and posterior), coracoclavicular ligaments (conoid and trapezium), insertions of the deltoid and trapezius muscle to the acromial end of the clavicle and capsular ligament of the sternoclavicular joint [5]. AC joint dislocation of Rockwood type II-III, chronic dislocations and horizontal instability after conservative treatment and operative treatment limited to the reconstruction of the coracoclavicular ligaments are very difficult to diagnose and treat [6]. Injuries to the AC joint still represent a diagnostic challenge for most shoulder surgeons.
Clinical and instrumental diagnostic methods appear quite simple and well-established. However, for various reasons, orthopedic surgeons often have to treat patients with complications such as AC arthritis, acromion osteolysis or ossification of the coracoclavicular ligament complex, which are quite often irreversible and lead to dysfunction of the shoulder joint complex [7,8].
Modern radiological diagnostics, using a vast array of methods such as conventional radiographs, ultrasound, CT, MRI, etc., are an essential tool for confirming a diagnosis. Radiography is the “gold standard” and is primarily useful for diagnosing the sequelae of injury and degenerative joint disease. X-ray criteria of AC joint dislocation have been sufficiently studied. Still, the clinical evaluation and possibilities of additional non-invasive instrumental diagnostics, such as CT, MRI and ultrasound, in the diagnosis of compound cases need to be investigated [9]. The aim of this article is to show that, although a gold standard to investigate and diagnose acute AC joint dislocation does not currently exist, there are best practices in diagnosis and, in turn, complete and early diagnosis of acromioclavicular dislocation allows for a differentiated approach to surgical treatment tactics, preventing complications that could occur, and fully restoring the function of the injured shoulder joint.
MATERIALS AND METHODS
A retrospective study was performed of 152 patients with traumatic shoulder pathology who were diagnosed and treated at the Department of Microsurgery and Reconstructive-Recovery Surgery of Upper Limb at the SI Institute of Traumatology and Orthopedics by NAMS of Ukraine between January 2010 and July 2020. The local Ethics Committee approved the study's design and written informed consent was obtained from all participants before enrolment. The patients were divided into two groups: Group I of 102 patients (67%) with acromioclavicular joint dislocation, mean age 34 years (range 20 to 68 years), mostly men – 100 (98%), and Group II of 50 patients (33%) with a partial tear of the rotator cuff, mean age 44 years (range 16 to 76 years), mostly men – 36 (72%). The diagnosis was verified intraoperatively in all patients. AC joint dislocation was classified according to the Rockwood classification, which is based on the injury's anatomical and radiological aspects and includes six types of injury [10].
Patients were examined using clinical and instrumental diagnostic methods, including specific provocative tests, i.e., the piano-key test, Paxinos test, crossbody adduction test and active compression test [9]. Radiographs were obtained in the Zanca view [11] (anteroposterior view with 10–15° cephalic beam inclination), axillary view and Alexander view [12]. Ultrasound examination was performed using PhilipsXD 11 and SiemensAT 3500 stationary systems, with a 7.5–11 MHz linear high-frequency probe in a “superficial musculocutaneous” mode according to a standard protocol. The contralateral AC joint was used as a control during the ultrasound examination. MRI examination of the shoulder and AC joint was performed on ≥ 1,5 T MRI scanner in sagittal, coronal, and axial Т1, Т2, PD and PD (Fat-Sat) views and sequences. CT examination of the shoulder and AC joint was conducted on a 16-slice MDCT scanner using multiplane (multiplanar) reconstruction (MPR) and 3D-reconstruction.
Statistical analysis was performed using STATISTICA 12.0 (StatSoft Inc. USA) and Microsoft Excel. A p-value < 0.05 was considered statistically significant [13]. Firstly, we determined true-positive, truenegative, false-positive, and false-negative items and then calculated all indices. Study data were evaluated using standard descriptive statistical markers for the evaluation of diagnostic tests: accuracy (overall probability that a patient is correctly classified), sensitivity (probability that a test result will be positive when the injury is present [true positive rate]), specificity (probability that a test result will be negative when the injury is not present [true negative rate]), where these markers are of diagnostic value if they are > 75%, as well as Positive Likelihood Ratio (PLR, ratio between the probability of a positive test result given the presence of injury and the probability of a positive test result given the absence of in jury), Negative Likelihood Ratio (NLR, ratio between the probability of a negative test result given the presence of injury and the probability of a negative test result given the absence of injury), Positive Predictive Value (PPV, probability that injury is present when the test is positive), and Negative Predictive Value (NPV, probability that injury is not present when the test is negative) with their 95% confidence intervals (95% CI). We categorized the diagnostic accuracy indices (PPV and NPV) as good (>0.8), acceptable (0.6-0.8), and weak (lower than 0.6). Categorization of the likelihood ratios was as follows: values of PLR greater than 10/NLR less than 0.1 were interpreted as a large and often conclusive in crease/decrease in the probability of injury; values of PLR between 5 and 10/NLR between 0.2 and 0.1 were interpreted as a moderate increase/decrease in the probability of injury; values of PLR from 2 to 5/NLR from 0.5 to 0.2 were assumed to indicate small (but sometimes important) shifts in the probability of injury; and likelihood ratios between 0.5 and 2 were assumed to represent small and rarely important changes in probability [14,15].
RESULTS
Modern clinical and instrumental diagnostic methods comprise a large number of techniques, but no single algorithm for diagnosing injury to the AC joint has been described.
Classification
Before the patients were transferred to our center, the types of AC joint injury were categorized as follows: 17 patients (16.6%) with AC joint dislocation according to Tossy classification, 32 patients (31.4%) by Rockwood classification, and the type of injury was not established in 53 patients (51.9%). Following a set of clinical and instrumental examinations at our center, patients were distributed according to Rockwood’s classification: type III injuries were diagnosed in 29 patients (28.4%), type IV in 4 patients (3.9%), type V in 68 patients (66.6%), and type VI in 1 patient (0.9%).
Physical examination
Parameters of clinical tests were determined in patients of Groups I and II (151 patients, 99.3%). A feature of this study was to determine the characteristics of specific provocative tests most commonly employed to identify injury to the AC joint according to the type of dislocation (Table 1).
Clinical examination is particularly useful for localizing a patient’s pain to a specific joint and the musculoskeletal structure involved. A 100% accurate, sensitive, and specific clinical test for the diagnosis of AC joint dislocation was not found in our study. Thus, instrumental diagnostics are mandatory.
X-ray examination
X-ray examinations of the patients from the first group involved the Zanca view (102 patients, 100%), axillary view (34 patients, 33%) and Alexander view (47 patients, 46%). In most cases (82%), previous management had included only one x-ray view (Tab. 2).
Tab. 1. Characteristics of specific provocative tests for AC joint dislocation by type of injury

Tab. 2. Characteristics of X-ray examination of patients with AC joint dislocation by type of injury

Analysis of the sensitivity and specificity of conventional radiographs of patients with AC joint dislocation found that radiography of the shoulder joint in the axillary view offers 100% sensitivity for detecting Rockwood type IV and VI (Fig. 1) dislocation. These dislocations result from high-energy trauma and are easily diagnosed by performing a specific X-ray view. The Zanca view is also highly sensitive for Rockwood type V and the Alexander view for Rockwood type III and V dislocations [16,17].
Ultrasound examination
Ultrasound examination was performed in 54 patients (52.9%) of Group I and 42 patients (84%) of Group II. The method's accuracy in the group of AC joint dislocation was 95%, with a sensitivity of 96% and a specificity of 93%. PLR 95% CI was 13.48 (4.53-40.17); this highly positive result indicates a large and often convincing increase in the probability of detecting patients with AC joint dislocation. NLR 95% CI was 0.04 (0.01-0.16) – a negative result of an ultrasound examination indicates a high probability of absence of AC joint dislocation. PPV 95% CI was 0.94 (0.85-0.98), indicating a very high correlation between a positive result and the presence of dislocation. NPV 95% CI = 0.95 (0.85-0.98) shows a very high correlation of a negative result of this method and the absence of AC joint dislocation.

Fig. 1 A – Zanca view x-ray of the AC joint: Rockwood type VI dislocation, B – axillary view x-ray of AC joint: Rockwood type IV

Fig. 2. Ultrasonographic examination of the AC joint: A – distance between the upper border of acromion and clavicle, vertical displacement of the acromial end of the clavicle in the frontal view, B – distance between the anterior border of acromion and clavicle, horizontal instability in axial view, C – distance between the upper border of the coracoid and lower border of clavicle, vertical instability
In our study (Fig. 2), vertical instability of the AC joint was determined in the frontal view: the mean distance between the upper border of the acromion process and the upper border of the acromial end of the clavicle was 14.4 ± 5.3 mm on the side of injury and 3.1 ± 1.1 mm on the contralateral side (p < 0.05). Additionally, a provocative test was performed where the distance between the upper border of the acromial process and the upper border of the acromial end of the clavicle on the side of the injury was measured during the piano-key test. On the injured side, the mean distance was 4.06 ± 1.4 mm, while on the contralateral side it was 3.4 ± 0.9 mm. (p = 0.001).
Horizontal instability of the AC joint was determined in the axial view: the mean distance from the anterior border of the acromial process to the anterior border of the acromial end of the clavicle was 3.5 ± 1.1 mm on the side of injury and 2.8 ± 0.7 mm in the contralateral joint (p < 0.05). Additionally, a provocative test was performed where the distance from the anterior border of the acromial process to the anterior border of the acromial end of the clavicle on the side of injury was measured during the Paxinos test. On the injured side, the mean distance was 8.1 ± 1.7 mm, and on the contralateral side it was 3.6 ± 0.5 mm (p < 0.05). Avulsion of the deltoid muscle insertion to the acromial end of the clavicle was diagnosed in 42 patients (77%) (8.6 ± 2.3 mm wide), and trapezius muscle avulsion was diagnosed in 31 (57%) (5.3 ± 1.4 mm wide).
The coracoclavicular distance was determined in the sagittal view. The mean distance between the most superior border of the coracoid process and the clavicle's inferior border was 23.6 ± 4.1 mm on the injured side and 11.5 ± 1.7 mm on the contralateral side (p < 0.05).
Additionally, the sternoclavicular joint was examined. The mean distance between the upper border of the clavicle and the upper border of the sternum was 6.1 ± 3.5 mm from the injured side and 3.1 ± 1.2 mm from the contralateral side (p < 0.05). Such changes are caused by injury to the ligaments of the sternoclavicular joint (anterior sternoclavicular ligament and costoclavicular ligament) due to elevation and rotation of the clavicle [18].
MRI
MRI scans were obtained for 26 patients (26%) in Group I and 50 patients (100%) in Group II. The accuracy of the method in the group of AC joint dislocation was 97%, with a sensitivity of 96% and a specificity of 98%. PLR 95% CI was 48.08 (6.90-335.17); this highly positive result indicates a large and often convincing increase in the probability of detecting patients with dislocation of the acromial end of the clavicle. NLR 95% CI was 0.04 (0.01-0.27) – a negative result for MRI indicates a high probability of absence of AC joint dislocation. PPV 95% CI = 0.96 (0.78-0.99) indicates a very high correlation of a positive test result and the presence of dislocation. NPV 95% CI = 0.98 (0.88-1.0) indicates a very high correlation a negative result and the absence of AC joint dislocation.
In the coronal view (Fig. 3), we examined the acromioclavicular distance in the frontal plane.

Fig. 3 A – vertical displacement of the AC joint, the distance between the upper and lower border of acromion and clavicle in the coronal plane, B – the distance between the upper border of the coracoid and lower border of clavicle, injury to coracoclavicular ligaments in the coronal plane, C – distance between the upper border of the coracoid and lower border of clavicle, injury to coracoclavicular ligaments in the sagittal plane, D – distance between the anterior and posterior border of acromion and clavicle in axial view, injury to the anterior and posterior AC joint ligament, hemarthrosis
The mean distance between the upper border of the acromion and the upper border of the acromial end of the clavicle was 12.6 ± 4.5 mm, and the mean distance between the lower border of the acromion and the lower border of the acromial end of the clavicle was 9.5 ± 4.1 mm. The mean coracoclavicular distance was 14.9 ± 5.6 mm. Injury to the lower and upper acromioclavicular ligament was identified in 24 patients (92%), intra-articular disc injury in 14 patients (53%), and injury to the conoid ligament in 25 patients (96%) and trapezoid ligament in 21 patients (81%).
In the axial view, we determined the mean distance from the anterior border of the acromial process to the anterior border of the acromial end of the clavicle on the side of injury: it was 10.1 ± 3.5 mm. The mean distance between the posterior border of the acromion process and the posterior border of the acromial end of the clavicle was 6.5 ± 3.1 mm.
Injury to the anterior acromioclavicular ligament was noted in 24 patients (92%), posterior acromioclavicular ligament was injured in 20 patients (77%), and the intra-articular disc in 16 patients (62%), detachment of the deltoid muscle was seen in 17 patients (65%) and trapezius muscle in 19 patients (73%) from the acromial end of the clavicle.
In the sagittal view, we determined the mean coracoclavicular distance to be 13.9 ± 3.2 mm, and found injury to the conoid ligament in 25 patients (96%) and to the trapezoid ligament in 21 patients (81%).
MRI examination of 26 patients (100%) revealed associated injuries of the shoulder joint in the form of a SLAP lesion (18 patients, 69%), biceps tendinitis (22 patients, 85%), partial rotator cuff tear (7 patients, 27%), biceps pulley lesion (7.7%), distal clavicular osteolysis (4 patients, 15%). They were confirmed intraoperatively and required an additional repair procedure. After MRI examinations of the shoulder and AC joint, the type of dislocation according to the Rockwood classification was changed in 8 patients (5.2%).
Computed tomography
CT examination was performed in 12 patients (12%) of Group I and 4 patients (8%) of Group II. The method's accuracy in determining the AC joint dislocation was 81%, sensitivity was 83%, and specificity was 75%. PLR 95% CI = 3.3 (0.6-18.54) is a highly positive result that indicates a large and often convincing increase in the probability of detecting patients with AC joint dislocation. NLR 95% CI was 0,22 (0.06-0.89) – a negative result for CT testifies to the high probability of absence of AC joint dislocation, PPV 95% CI = 0,9 (0,64-0,98) indicates a very high correlation of a positive test result and the presence of dislocation. NPV 95% CI = 0.6 (0.27-0.85) indicates a very high correlation of a negative result and the absence of AC joint dislocation.
In the coronal view, we examined the acromioclavicular distance in the frontal plane: the mean distance between the upper border of the acromion and the upper border of the acromial end of the clavicle was 12.9 ± 2.8 mm, compared to 4.9 ± 1.5 mm on the contralateral side (p < 0.05), the mean distance between the lower border of the acromion and the lower border of the acromial end of the clavicle was 9.5 ± 3.3 mm, compared to 2.6 ± 0.9 mm on the contralateral side (p < 0.05). The mean coracoclavicular distance was 13.5 ± 3.5 mm, compared to 5.9 ± 1.6 mm on the contralateral side (p < 0.05). In the axial view, we determined the mean distance between the anterior border of the acromial process and the anterior border of the acromial end of the clavicle on the side of injury, which was 13.3 ± 2.3 mm. On the contralateral side, it was 2.6 ± 0.9 mm (p < 0.05). The mean distance between the posterior border of the acromion process and the posterior border of the acromial end of the clavicle was 9.6 ± 3.0 mm, compared to 5.2 ± 2.4 mm on the contralateral side (p < 0.05). The mean value of AС joint angles on the injury side was 24.30± 6.60 and on the contralateral side it was 18.90± 3.70 (p = 0.023).
Type IV of AC joint dislocation by Rockwood was diagnosed in 1 patient (1%). It was not identified on standard anteroposterior plain radiographs of the AC joint (Fig. 4).

Fig. 4. CT of the shoulder joint (A - Rockwood type IV AC joint dislocation in the axial plane, B – AC joint dislocation is not detected in the coronal plane)
The following associated injuries of the shoulder joint were found during CT examination: os acromiale was diagnosed in 2 patients (2%) (Fig. 5); 1 patient (1%) post conservative treatment was diagnosed with ossification of the coracoclavicular and coracoacromial ligament of the AC joint, which influenced the tactic of surgical treatment (Fig. 6). In 5 patients, the diagnosis and the type of AC joint dislocation coincided.

Fig. 5. CT of the shoulder joint (A – dislocation of the acromial end of the clavicle in the vertical plane, B – Os acromiale condyle of the scapula)

Fig. 6. Ossification of coracoclavicular and coracoacromial ligaments (A – frontal view, B – posterior view)
DISCUSSION
The study summarizes the methodology of clinical and instrumental methods available for the preoperative work-up of patients with acromioclavicular joint dislocation who underwent operative treatment in our department over the past 10 years. It is shown that high-quality preoperative examination of patients is the key to successful surgical treatment, postoperative rehabilitation, and recovery.
The physical examination of acute AC joint dislocation is well studied and described in many guidelines, textbooks, and scientific articles [19-26]. Chronopoulos et al. reported a sensitivity of 77% for the cross-body adduction test, 72% for the AC resistance test, and 41% for the active compression test; the combination of all 3 tests showed a specificity of 95% [27]. The combination of the Paxinos sign and Hawkins–Kennedy test has a sensitivity of 93% if both special tests are negative; the combination of O'Brien's Test and AC joint tenderness demonstrated the greatest specificity (96.7%), although it was the combination of Paxinos sign and O'Brien's test that had the highest calculated positive likelihood ratio of 2.71 [28]. According to our study results, no clinical test had 100% accuracy, sensitivity and specificity for detecting AC joint injuries. In patients with Rockwood type III AC joint dislocation, the highest accuracy of 77% was revealed for the piano-key test and Paxinos test, while the cross-body adduction test had 65% sensitivity, and the piano-key test had 88% specificity. In patients with Rockwood type IV AC joint dislocation the piano-key test also had 87% accuracy, and this test, the Paxinos test and the cross-body adduction test had 75% sensitivity; the piano-key test also had 88% specificity. In patients with Rockwood type V AC joint dislocation, the Paxinos test had 89% accuracy and 91% sensitivity and the piano-key test had 88% specificity. An explanation for these findings may be that at the time of injury, it is not always possible to conduct clinical testing of patients due to low pain intensity or in patients with increased subcutaneous fat [29]. If patients do not report immediately after the injury and soft tissue edema increases, the identification of shoulder joint anatomical landmarks becomes difficult. Also, the lack of a specific test for AC joint dislocation is due to the presence of simultaneous concomitant injuries in the shoulder joint.
Developed by Rockwood et al. in 1984, his six-type classification system is the most common and popular classification used for acromioclavicular joint dislocations. Since then, numerous modifications of the classification system have been suggested by various authors. In 2014, the Upper Extremity Committee of ISAKOS subdivided Rockwood’s type III of AC joint dislocation into two types after x-ray examinations in specific view (cross-body stress view), namely, type ІІІ А of stable injures that should be evaluated for conservative treatment and type ІІІ В of unstable injures that should be evaluated for operative treatment, but it is unclear to what extent this subdivision predicts treatment outcomes [30, 31]. De Rooij et al. showed in his survey significant individual variation with regard to diagnosis of AC joint dislocation, with 65 (61%) respondents using the Rockwood classification, and 41 (39%) using the Tossy classification [32]. In our study, 17 patients (16.6%) were classified according to the Tossy classification,32 patients (31.4%) were classified according to the Rockwood classification, and, in 53 patients, the type of injury was not established (51.9%) during earlier management.
Plain radiographs are a standard examination for patients with AC joint injury, as based on the original descriptions by Tossy et al., Allman and Rockwood et al.
A national survey in the Netherlands shows that the diagnosis of AC joint dislocation is mainly based on a combination of physical examination and radiographs; 89% of respondents used anteroposterior and axial radiographs, 33% used Zanca view radiographs, and 15% used weight-bearing radiographs. For decades, surgeons worldwide have debated whether weighted or non-weighted views diagnose AC joint dislocations effectively [33]. Bossart et al. presented 83 pairs of radiographs with and without weights obtained as part of work-up for AC joint dislocation. In only three cases (4%) did the weights cause the coracoclavicular distance on the injured side to increase, thereby revealing a grade 3 injury not evident on plain radiographs [34]. In our study, after performing additional X-ray examination (axillary and Alexander view), the type of AC joint dislocation was changed from Rockwood type II/III to type IV in 3 patients (2.9%), from type II to III in 5 patients (4.9%), and from type III to V in 2 patients (1.9%). The absence of 100% sensitive and specific radiographs for all AC joint dislocation types requires an X-ray examination in at least three views.
Depending on the severity of the injury, the coracoclavicular ligaments can be stretched [35], partially torn, or completely torn; an ultrasound examination can evaluate their contribution to AC joint injury diagnosis. In a human cadaveric study, Gerhard Martin Hobusch et al. determined that horizontal displacement in the AC joint was 1.3 ± 0.9 mm with intact ligaments, 1.4 ± 1.2 mm after transecting the AC ligaments, and 1.9 ± 1.3 mm after additionally transecting the CC ligament. The joint space was 3.3 ± 1.1 mm with intact ligaments, 4.1 ± 1.8 mm in an iatrogenic Rockwood type II injury, and 5.3 ± 3.3 mm in an iatrogenic Rockwood type III injury [36]. Heers et al. performed ultrasound examinations in 13 cadaveric acromioclavicular joints. The mean sonographic width of the joint space was 3.9 mm ± 1.7 mm and the distance from the joint space to the capsular insertions on the clavicle and on the acromion was 4.4 ± 1.4 mm and 5.3 ± 2 mm, respectively [37]. In another study, an ultrasound examination was developed and tested for its ability to detect ligament in jury and mean distance in the AC joint in the horizontal [38] and vertical plane, measure distance between the coracoid process and clavicle, to detect dynamic instability with provocative tests (piano-key test and Paxinos test) in the vertical and horizontal planes, identify detachment of the deltoid and trapezius muscles from the acromial end of the clavicle and injury to the capsular ligament of the sternoclavicular joint, and compare the indicators with the contralateral intact joint.
MRI is optimal for evaluating soft tissue injuries, occult fractures, articular cartilage damage, synovitis, and there is no risk of radiation exposure to the patient, but it is not a routine method for diagnosing AC joint dislocation [39]. However, there is a growing interest in and popularization of the use of this method for assessing AC and coracoclavicular ligamentous injury [40,41]. Kaywan Izadpanah et al. described a new method: stress MRI facilitates the acquisition of morphologic and functional information on acute ACJ injuries; it helps to distinguish between partial and complete ligament tears. In chronic ACJ injuries, it provides functional information about ligament regrinds [42]. In our study, in most patients with acute AC joint dislocation, MRI scans revealed injury to both coracoclavicular ligaments (96% for conoid ligament and 81% for trapezoid ligament), detachment of the deltoid muscle (65%) and trapezius muscle (73%), injury to both acromioclavicular ligaments. Stress MRI should be used as an additional option in difficult cases. Jensen et al. identified one or more concomitant glenohumeral pathologies in 201 patients (53%) who underwent arthroscopically-assisted stabilization of acromioclavicular joint dislocation of Rockwood type III and V. We observed concomitant glenohumeral pathologies (SLAP lesion, biceps tendinitis, partial rotator cuff tear, biceps pulley lesion, os acromiale, distal clavicular osteolysis) in 22 patients (85%). MRI should be mandatory in examination of patients with AC joint injury to choose the tactics of surgical intervention, i.e. an open (mini-open) procedure only on the AC joint or arthroscopically-assisted procedure to treat concomitant glenohumeral pathologies.
CT imaging is not a routine evaluation of AC joint dislocation. Nouh MR et al. determined the morphometric and biometric measurements of the typical AC joint in vivo on a multidetector CT device: anterior and posterior axial AC joint distances were 0.59± 0.27 cm and 0.26 ± 0.11 cm; the coracoclavicular distance was 0.73 ± 0.41 cm; the AC angle was 26.550 ± 14.71 [43]. David R Dyer et al. described the case of a 21-year-old female pedestrian involved in a motor vehicle accident that presented 4 months post-injury with unresolved shoulder pain. However, acute trauma X-ray and CT showed no shoulder abnormality. Repeat plain radiographs showed a moderately increased coracoclavicular distance, an ultrasound examination showed a partial rotator cuff tear and disruption of the AC joint, and a MRI examination showed mild AC joint disruption. Dynamic 4D CT showed a significant translation of the AC joint in multiple planes, which changed future management. With a wide field of view, dynamic 4D CT is an accurate and quick modality to diagnose acute and chronic AC joint injury [42, 44-50]. Given the hazards of ionizing radiation, it is pertinent to investigate diagnostic examinations using non-hazardous imaging modalities to examine the acromioclavicular joint. The frequently sports-related nature of the injury often means that the patient is a young adult.
Delayed and incomplete diagnosis is one of the main reasons for unsatisfactory treatment outcomes for ACC dislocations. To optimize the diagnosis of shoulder joint lesions, we analyzed the available examination methods, and the most informative of them were selected, on the basis of which a set of diagnostic measures was proposed that maximally reflects the condition of the joint without resorting to invasive research methods. According to the results of the study, no clinical test can indicate AC joint dislocation with 100% sensitivity and specificity. Determination of sensitivity and specificity of X-ray examination revealed that no specific X-ray view can detect type III and V of dislocation with 100% accuracy. The accuracy and sensitivity of ultrasound, MRI, and CT are high.
A gold standard for investigating and diagnosing acute AC joint dislocation does not currently exist. There is currently no consensus on a protocol to view acute AC joint injuries. Complete and timely early diagnosis of acromioclavicular dislocation allows for a differentiated approach to surgical treatment tactics, preventing possible complications and fully restoring the function of the injured shoulder joint [51,52].
CONCLUSIONS
1. Determination of the sensitivity and specificity of the X-ray examination revealed the absence of a 100% effective X-ray view for type III and V AC joint dislocation.
2. The accuracy and sensitivity of the ultrasound, MRI, and CT examinations are high.
3. There is currently no consensus on a protocol to view acute AC joint injuries.
4. Complete and timely early diagnosis of acromioclavicular dislocation allows for a differentiated approach to surgical treatment tactics, preventing possible complications and restoring the function of the injured shoulder joint to the fullest extent.
REFERENCES
1. Tauber M, Koller H, Hitzl W, Resch H. Dynamic radiologic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med 2010; 38(6): 1188-95.
2. Martetschläger F, Kraus N, Scheibel M, Streich J, Venjakob A, Maier D. The Diagnosis and Treatment of Acute Dislocation of the Acromioclavicular Joint. Deutsches Arzteblatt International 2019; 116(6): 89-95.
3. Cook JB, Tokish JM. Surgical Management of Acromioclavicular Dislocations. Clin Sports Med 2014; 33(4): 721-37. doi: 10.1016/j.csm.2014.06.009.
4. Kazda S, Pasa L, Pokorny V. Clinical outcomes of surgical management of acromioclavicular dislocation with and without ligament suturing. Rozhl Chir 2011; 90(10): 561-4.
5. Keener JD. Acromioclavicular Joint Anatomy and Biomechanics. Operative Techniques in Sports Medicine 2014; 22(3): 210-3.
6. Malahias MA, Sarlikiotis T, Brilakis E, Gerogiannis D, Avramidis G, Antonogiannakis E. The clinical outcome of the ‘Surgilig’technique for the reconstruction of acromioclavicular dislocations: A systematic review. J. Orthop. 2020; 18: 126-31.
7. Boffano M, Mortera S, Wafa D, Piana R. The surgical treatment of acromioclavicular joint injuries. EFORT Open Reviews 2017; 2(10): 432-7.
8. Aagesen AL, Melek M. Choosing the right diagnostic imaging modality in musculoskeletal diagnosis. Primary Care: Clinics in Office Practice 2013; 40(4): 849-61.
9. Rockwood CA Jr, Matsen FA, Wirth MA, Lippitt SB, Fehringer EV, Sperling JW. Rockwood and Matsen's the shoulder, Fifth Edition. Philadelphia, PA: Elsevier; 2018.
10. Zanca P. Shoulder pain: involvement of the acromioclavicular joint. Analysis of 1,000 cases. The American journal of roentgenology, radium therapy, and nuclear medicine 1971; 112(3): 493-506.
11. Chronopoulos E, Kim TK, Park HB, Ashenbrenner D, McFarland EG. Diagnostic Value of Physical Tests for Isolated Chronic Acromioclavicular Lesions. American Journal of Sports Medicine 2004; 32(3): 655-61.
12. Krill MK, Rosas S, Kwon K, Dakkak A, Nwachukwu BUU, McCormick F. A concise evidence-based physical examination for diagnosis of acromioclavicular joint pathology: a systematic review. The Physician and sportsmedicine 2018; 46(1): 98-104.
13. Tauber M. Management of acute acromioclavicular joint dislocations: Current concepts. Archives of Orthopaedic and Trauma Surgery 2013; 133(7): 985-95.
14. Rooij PPD, Van Lieshout EMM, Schurink IJ, Verhofstad MHJ. ACJ injury study group, Current practice in the management of acromioclavicular joint. European Journal of Trauma and Emergency Surgery 2020.
15. Bossart PJ, Joyce SM, Manaster BJ, Packer SM. Lack of efficacy of 'weighted' radiographs in diagnosing acute acromioclavicular separation. Annals of Emergency Medicine 1988; 17(1): 20-4.
16. Karargyris O, Murphy RJ, Arenas A, Bolliger L, Zumstein MA. Improved identification of unstable acromioclavicular joint injuries in a clinical population using the acromial center line to dorsal clavicle radiographic measurement. Journal of Shoulder and Elbow Surgery 2020; 5: 1-7.
17. Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 2011; 39(7): 1507-16.
18. Barnes CJ, Higgins LD, Major NM, Basamania CJ. Magnetic resonance imaging of the coracoclavicular ligaments: its role in defining pathoanatomy at the acromioclavicular joint. J Surg Orthop Adv 2004; 13(2): 69-75.
19. Alyas F, Curtis M, Speed C, Saifuddin A, Connell D. MR imaging appearances of acromioclavicular joint dislocation. Radiographics 2008; 28(2): 463-79.
20. Bathis H, Tingart M, Bouillon B, Tiling T. The status of therapy of acromioclavicular joint injury. Results of a survey of trauma surgery clinics in Germany. Unfallchirurg 2001; 104(10): 955-60.
21. Leidel BA, Braunstein V, Kirchhoff C, Pilotto S, Mutschler W, Biberthaler P. Consistency of long-term outcome of acute Rockwood grade III acromioclavicular joint separations after K-wire transfixation. J Trauma 2009; 66(6): 1666-71.
22. Martetschläger F, Kraus N, Scheibel M, Streich J, Venjakob A, Maier D. The Diagnosis and Treatment of Acute Dislocation of the Acromioclavicular Joint. Dtsch Arztebl Int. 2019; 116(6): 89-95.
23. Zumstein MA, Schiessl P, Ambuehl B, et al. New quantitative radiographic parameters for vertical and horizontal instability in acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc 2018; 26: 125-35.
24. Sirin E, Aydin N, Topkar O. Acromioclavicular joint injuries: diagnosis, classification and ligamentoplasty procedures. EFFORT Open Reviews 2018; 3(7): 426-33.
25. Moatshe G, Kruckeberg B, Chahla J, et al. Acromioclavicular and Coracoclavicular Ligament Reconstruction for Acromio - clavicular Joint Instability: A Systematic Review of Clinical and Radiographic Outcomes. The Journal of Arthroscopic and Related Surgery 2017; 1(1): 1-17.
26. Tang G, Zhang Y, Liu Y, Qin X, Hu J, Li X. Comparison of surgical and conservative treatment of Rockwood type-III acromioclavicular dislocation. Medicine (Baltimore) 2018; 97(4).
27. Zooker CC, Parks BG, White KL, Hinton RY. TightRope versus fiber mesh tape augmentation of acromioclavicular joint reconstruction: a biomechanical study. Am J Sports Med 2010; 38(6): 1204-8.
28. Assaghir YM. Outcome of exact anatomic repair and coracoclavicular cortical lag screw in acute acromioclavicular dislocations. J Trauma 2011; 71(3): E50-E4.
29. Grunau G, Linn S. Commentary: Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Frontiers in public health 2018; 6: 256.
30. Antonio GE, Cho JH, Chung CB, Trudell DJ, Resnick D. Pictorial essay. MR imaging appearance and classification of acromioclavicular joint injury. AJR Am J Roentgenol 2003; 180(4): 1103-10.
31. Ringenberg JD, Foughty Z, Hall AD, Aldridge JM, Wilson JB, Kuremsky MA. Interobserver and intraobserver reliability of radiographic classifcation of acromioclavicular joint dislocations. J Shoulder Elbow Surg 2018; 27(3): 538-44.
32. Hobusch GM, Fellinger K, Schoster T, Lang S, Windhager R, Sabeti-Aschraf M. Ultrasound of horizontal instability of the acromioclavicular joint: A simple and reliable test based on a cadaveric study. Wiener klinische Wochenschrift 2019; 131(3-4): 81-6.
33. Rosso C, Martetschläger F, Saccomanno MF, Voss A, Lacheta L. High degree of consensus achieved regarding diagnosis and treatment of acromioclavicular joint instability among ESA-ESSKA members. Knee Surgery, Sports Traumatology, Arthroscopy 2020. https://doi.org/10.1007/s00167-020-06286-w
34. Heer G, Götz J, Anders S, Hedtmann A. Sonometrie des Akromioklavikulargelenkes – Korrelation anatomischer und sonographischer Befunde. Sonometrie des Akromioklavikulargelenkes – Korrelation anatomis. European Journal of Ultrasound 2006; 27(6): 549-52.
35. Smith TO, Chester R, Pearse EO, Hing CB. Operative versus non-operative management following Rockwood grade III acromioclavicular separation: a meta-analysis of the current evidence base. J Orthop Traumatol 2011; 12(1): 19-27.
36. Izadpanah K, Winterer J, Vicari M, et al. A Stress MRI of the Shoulder for Evaluation of Ligamentous Stabilizers in Acute and Chronic Acromioclavicular Joint Instabilities. Journal of Magnetic Resonance Imaging 2013; 37(6): 1486-92.
37. Mohamed RN, Doweidar A, Aziz Amr HEl, Refae DEl, Ashry M, Kandri SAl. The Normal Acromioclavicular Joint: An In Vivo Multidetector CT (MDCT) Morphometric and Biometric Cross Sectional Feasibility Study. OMICS journal of radiology 2017; 6.
38. Martetschläger F, Kraus N, Scheibel M, Streich J. The Diagnosis and Treatment of Acute Dislocation of the Acromioclavicular Joint. Deutsches Aerzteblatt International 2019; 116. Doi:10.3238/arztebl.2019.0089.
39. Kienast B, Thietje R, Queitsch C, Gille J, Schulz AP, Meiners J. Mid-term results after operative treatment of Rockwood grade III-V acromioclavicular joint dislocations with an AC-hook-plate. Eur J Med Res 2011; 16(2): 52-6.
40. Emery R. Acromioclavicular and sternoclavicular joints. In: Copeland S (ed) Shoulder surgery. London: WB Saunders; 1997.
41. Phadke A, Bakti N, Bawale R, Singh B. Current concepts in management of ACJ injuries. J Clin Orthop Trauma 2019; 10(3): 480-5.
42. Dyer DR, Troupis JM, Moaveni AK. Wide field of view CT and acromioclavicular joint instability: A technical innovation. Journal of Medical Imaging and Radiation Oncology 2015; 59(3): 326-30.
43. Doroudi T, Kolivand P, Divanbeigi A, et al. Comparing Diagnostic Accuracy of Direct Questioning Versus Schematic Evaluation of Chronic Pain Localization. Acta clinica Croatica 2017; 56(4): 689-97.
44. Granville-Chapman J, Torrance E, Rashid A. The Rockwood classification in acute acromioclavicular joint injury does not correlate with symptoms. Journal of Orthopaedic Surgery 2018; 26(2): 1-5.
45. Riand N, Sadowski C, Hoffmeyer P. Acute acromioclavicular dislocations. Acta Orthop Belg 1999; 65(4): 393-403.
46. Yewlett A, Dearden P, Ferran N. Acromioclavicular Joint Dislocation: Diagnosis and Management. Shoulder & Elbow 2017; 4(2): 81-6.
47. Nolte PC, Lacheta L, Dekker TJ, Elrick BP, Millett PJ. Optimal Management of Acromioclavicular Dislocation: Current Perspectives. Orthop Res Rev 2020; 12: 27-44.
48. Issa SP, Payan C, Le Hanneur M, Loriaut P, Boyer P. Arthroscopically assisted reduction of acute acromioclavicular joint dislocation using a single double-button device: Medium-term clinical and radiological outcomes. Orthopaedics & Traumatology: Surgery & Research 2018; 104(1): 33-8.
49. Muccioli M, Maria G, Manning C, et al. Acromioclavicular joint reconstruction with the LARS ligament in professional versus non-professional athletes. Knee Surg Sports Traumatol Arthrosc 2016; 24(6): 1961-7.
50. Bugelli G, Dell’Osso G, Ascione F, Gori E, Bottai V, Giannotti S. LARSTM in ACL reconstruction: Evaluation of 60 cases with 5–year minimum follow–up. Musculoskelet. Surg. 2017; 102(1). Doi: 10.1007/s12306-017-0499-3
51. Nascimento A, Claudio G. Functional and radiological evaluation of acute acromioclavicular dislocation treated with anchors without eyelet: comparison with other techniques. Rev. bras. ortop. 2016; 51(5). https://doi.org/10.1016/j.rboe.2016.08.015.
52. Maier D, Jaeger M, Reising K, et al. Injury patterns of the acromioclavicular ligament complex in acute acromioclavicular joint dislocations: a cross-sectional, fundamental study. BMC Musculoskelet Disord 2016; 17: 385.
- Tag:
- Complete and timely early diagnosis
- acromioclavicular dislocation
- Oleksii Dolhopolov
- joint dislocation
- X-ray
- MRI
- diagnostics
- sensitivity and specificity
- acromioclavicular joint
- outcomes